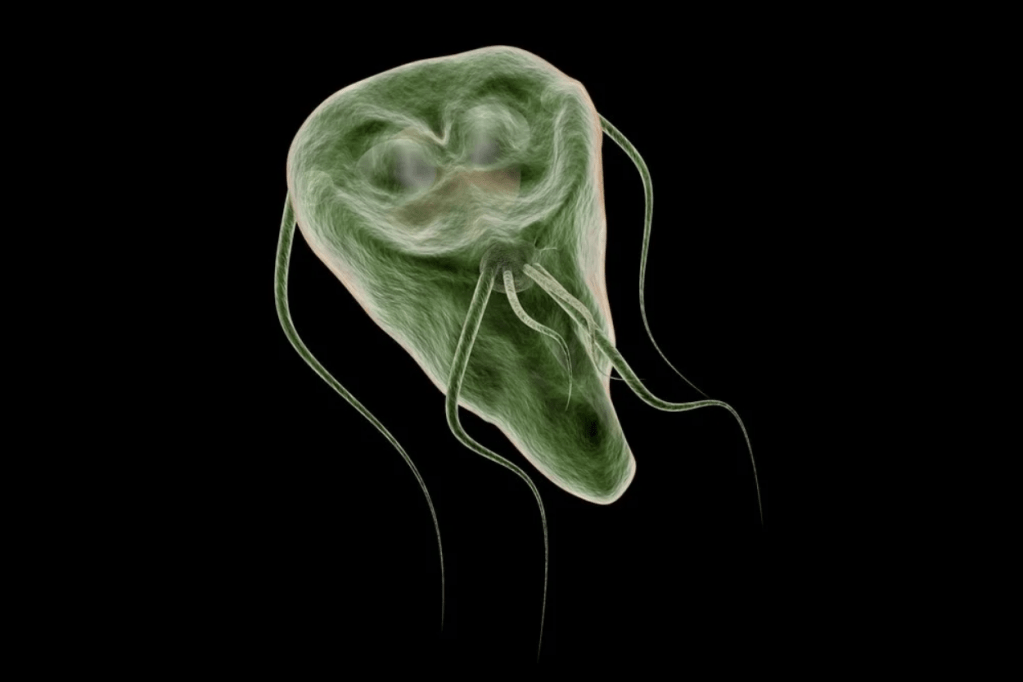
People who suffer from inflammatory bowel diseases (IBD) have a chronic illness often managed with a combination of medications, lifestyle changes, and surgeries. Unfortunately, there is no “one cure” for Crohn’s or ulcerative colitis, but specific treatments can help patients maintain their quality of life.
Prescriptions
There are many classes of drugs that can treat IBD, but consistency is vital. Doctors want to keep IBD sufferers in remission, which means not suffering from diarrhea and abdominal pain every day. Immune-modulating drugs work to control patients’ immune systems, suppressing flare-ups and keeping them under control.
Aminosalicylates (5-ASA)
Approved for Crohn’s:
• Flagyl (metronidazole)
• Cipro (ciprofloxacin)
Approved for Ulcerative Colitis:
• Asacol
• Azulfidine (sulfasalazine)
• Apriso
• Delzicol (mesalamine)
• Pentasa
• Lialda
• Colazal (balsalazide)
• Canasa (mesalamine suppositories)
• Rowasa (mesalamine enemas)
• Dipentum (olsalazine)
Antibiotics
Approved for Crohn’s:
• Flagyl (metronidazole)
• Cimzia (certolizumab pegol)
Biologics
Approved for Crohn’s:
• Humira (adalimumab)
• Entyvio (vedolizumab)
• Remicade (infliximab)
• Inflectra (infliximab-dyyb)
• Cimzia (certolizumab pegol)
• Tysabri (natalizumab)
• Stelara (ustekinumab)
Approved for Ulcerative Colitis:
• Remicade (infliximab)
• Entyvio (vedolizumab)
• Humira (adalimumab)
• Simponi (golimumab)
• Inflectra (infliximab-dyyb)
• Tysabri (natalizumab)
• Stelara (ustekinumab)
Over-the-Counter (OTC) Therapies
Thankfully, there are over-the-counter therapies that IBD patients can turn to when they need relief from symptoms without worrying about side effects. They include:
• Acetaminophen
• Fiber supplements
• Iron
• Anti-diarrheal medications
• Vitamin D
• Calcium
IBD patients have a lot of options when it comes to treatment. The two most common treatments for IBD include pharmaceuticals and surgery. Unfortunately, pharmaceuticals often include steroids, which may make your symptoms worse in the long run. Surgery, too, has its risks and complications.
Lifestyle
Good nutrition is imperative for managing Crohn’s disease and ulcerative colitis, but it can be difficult to stick to a healthy diet when you’re in pain.
Low-Residue Diet
Doctors may recommend a low-residue diet for those who have experienced bowel obstruction, chronic indigestion, or frequent bloating. In addition, if you have a narrowed bowel, you will need to change how you eat: avoid foods like popcorn and other high-fiber foods and focus on carbohydrate and fat-rich meals that will help keep sticky food moving through your digestive tract.
Enteral or Parenteral Nutrition
Enteral or parenteral nutrition is the only choice for patients who cannot eat by mouth. Some patients may need to take specialized formulas through a feeding tube, while others may need to be administered the formula through an IV. Doctors suggest parenteral nutrition for patients who are unable to eat enough calories to maintain their weight. The formula bypasses the gastrointestinal tract to go directly into the bloodstream.
Intravenous nutrition is an important part of Crohn’s disease treatment. It allows for the delivery of all the calories, electrolytes, minerals, proteins, fats, carbohydrates, vitamins, and other nutrients that a person with Crohn’s disease needs to be healthy. This is possible via an intravenous catheter.
Surgeries
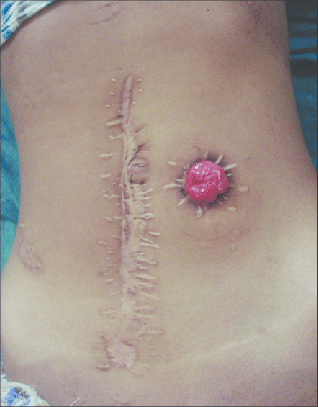
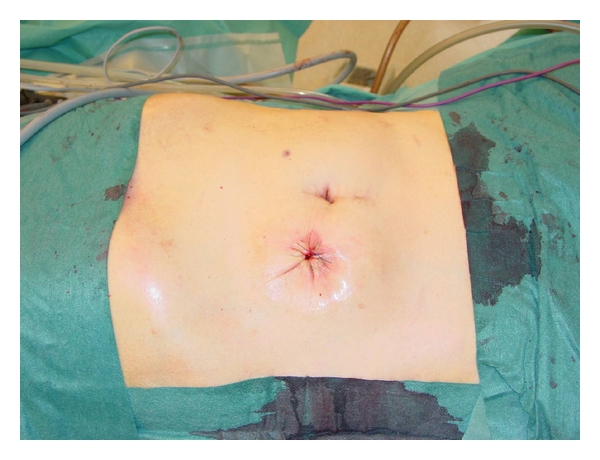
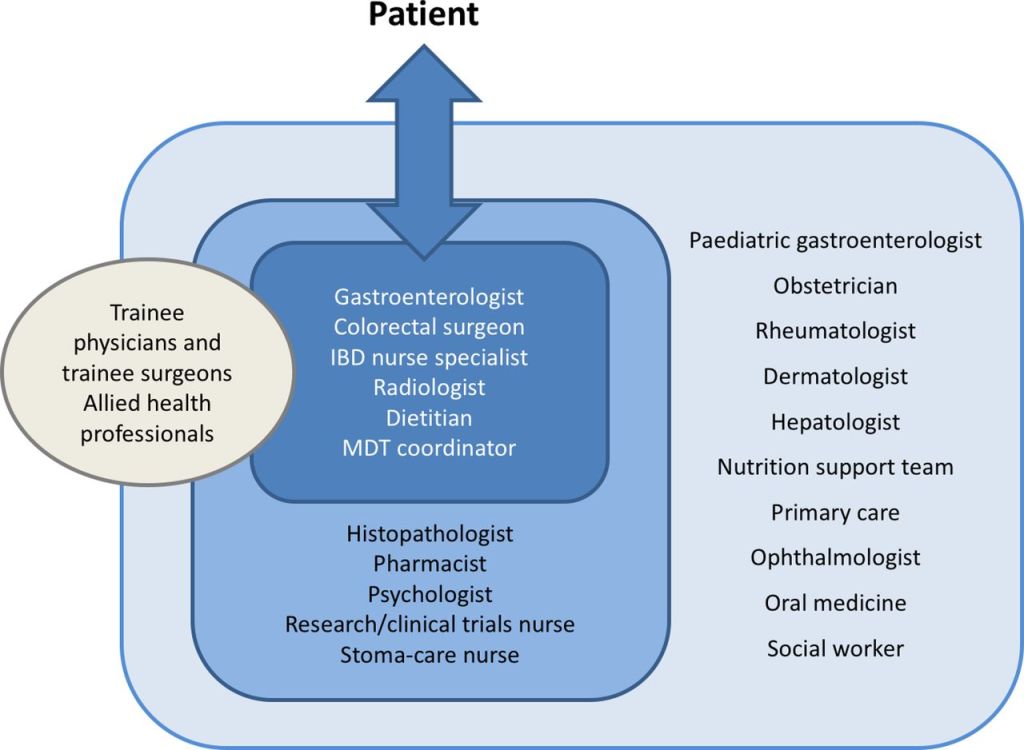
Patients can require surgeries to treat IBD — and different types of surgery are used to treat patients with Crohn’s disease and ulcerative colitis. In the case of Crohn’s, surgeons will often remove the diseased portions of the colon or rectum, while UC requires removal of intestines that the disease has damaged.
Procedures for Crohn’s Disease:
• Proctocolectomy (ileoanal anastomosis, straight pull-through)
• Resection
Procedures for Ulcerative Colitis:
• Proctocolectomy with the creation of an ileostomy
• Proctocolectomy with the creation of pelvic pouch (ileal pouch-anal anastomosis, IPAA)
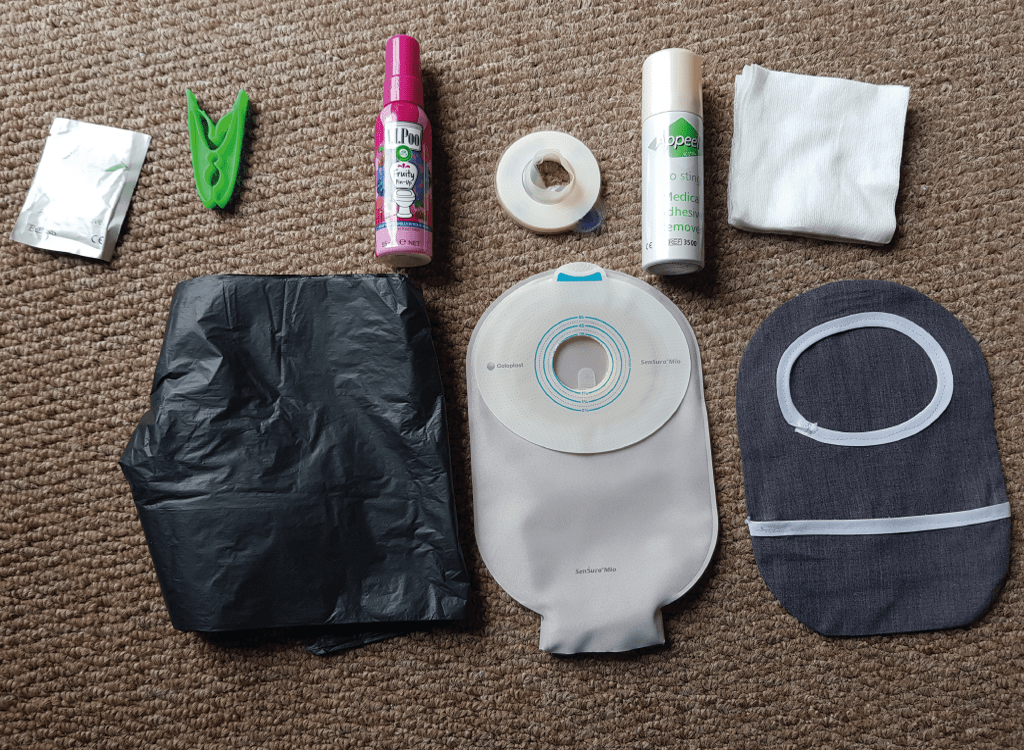
While these IBD surgeries are drastic measures, they dramatically improve a patient’s quality of life. While a partial or full ileostomy or colostomy is extreme, the newest therapies aim to minimize each surgery’s side effects and risks.

Thank you for reading this guide on inflammatory bowel disease treatment. We hope it helps you decide on the right course for your health and gives you peace of mind about what you need to do next.